According to a case report published in Pulmonary Circulation, immunotherapy, and chemotherapy used in concert with triple therapy may enhance clinical status and impact the effectiveness of treatment for pulmonary arterial hypertension (PAH).1.
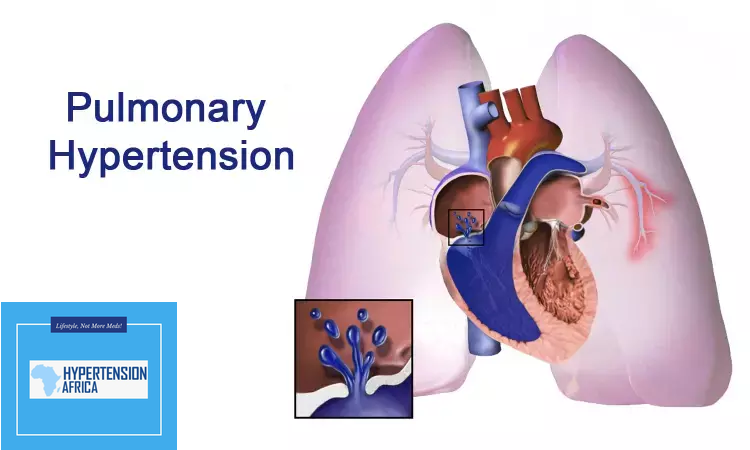
The rare, progressive disease, PAH, is characterized by pulmonary artery narrowing. When an artery narrows, the heart must work harder to pump blood to the lungs because this increases blood pressure in the arteries. Although the symptoms of PAH may not be severe at first, the added work progressively weakens the heart muscle. The illness may pose a serious risk to life in certain individuals.
The quality of life may be impacted by PAH medicines that are currently accessible, claim the authors.2. However, none address the important structural change known as vascular remodeling, which causes the pulmonary arteries to narrow.
The current study’s authors detailed the clinical development of an adult patient who benefited from dual therapy for lung cancer and PAH.1. They also talk about biological processes that could have aided in her treatment’s effectiveness.
Read Also: Smartphone app transforms blood pressure monitoring for underserved communities
PAH Treatment Course
The main complaints of a 52-year-old woman who had a history of ulcerative colitis, CREST scleroderma, connective tissue disease (CTD)–associated PAH, and interstitial lung disease were weariness and bone discomfort. She had been receiving PAH triple therapy for some years before the start of her visit in 2020.
The initial workup identified several hypermetabolic lesions in the liver (the largest measuring 2.8 cm with a standard uptake value of 43), bilateral ground glass interstitial opacities with areas of septal thickening, an incidental 4-cm left lower lobe nodular mass and osseous metastatic disease.
Poorly differentiated metastatic lung adenocarcinoma (stage 4) with 5% tumor cells expressing PD-L1 and negative for EGFR/ALK gene mutations was revealed by ultrasound-guided biopsy.
Initially, treating physicians thought that pembrolizumab plus carboplatin and pemetrexed would be the best course of treatment. However, the woman only took carboplatin and pemetrexed because doctors were worried that immunotherapy might make her scleroderma and interstitial lung disease worse. Following a well-tolerated first cycle, the doctors increased her dosage of pembrolizumab. Every three weeks, she had treatment.
Following a month of concurrent treatments, the patient had no symptoms. She was able to resume her teaching job once her 6-minute walk distance increased.
She saw six more months of clinical improvement. Improved cardiac output/cardiac index, a normal right atrium size, and somewhat reduced right ventricular (RV) function were all seen on echocardiograms. She did, however, later experience tiredness, dyspnea, and pancytopenia brought on by chemotherapy. She thereafter solely received pembrolizumab.
Pneumonitis forced the patient to stop receiving pembrolizumab, so they continued taking it for an additional five months. Importantly, the doctors discovered no evidence of active malignancy on PET/CT imaging at this time. Moreover, repeated surveillance PET/CT imaging over the next 18 months showed no evidence of cancer reoccurrence or metastatic illness.
Despite continuing her triple medication for PAH, her illness continued to worsen. Early in 2022, RV function was considerably reduced and there was considerable hypertrophy of the RV on echocardiograms. Due to severe right-sided cardiac failure and acute chronic respiratory failure, the patient passed dead in September 2022.
Biological Mechanisms May Influence PAH Status
The authors claim that tumor cells and pulmonary artery smooth muscle cells (PASMCs) have similar biological properties. They proposed that processes contributing to neoplastic lesions in malignancy may overlap with mechanisms contributing to plexiform lesions and several other cell types in PAH.
The autopsy demonstrated interstitial lung disease and significant enlargement of the PASMCs. However, there was no sign of lymphangitic carcinomatosis, infectious pneumonia, residual primary or metastatic disease, or pulmonary thromboembolism.
However, fibrous blockage of the pulmonary vein was revealed by lung tissue biopsies, which suggested the presence of pulmonary veno-occlusive disease (PVOD), an uncommon kind of pulmonary hypertension. The patient’s PAH may have gotten worse due to PVOD caused by the combination of immunotherapy and chemotherapy, according to the investigators’ theory.
Furthermore, they observed that her better pulmonary function coincided with an increase in the FOX01 transcription factor. The authors postulated that reverse remodeling, which is known to be regulated by FOX01 in cancer cells, might also exist in PASMCs.
Finally, they conjectured that the patient in question might have had underlying PVOD in addition to her scleroderma diagnosis. Thus, while its discontinuation made her situation worse, a combination of chemotherapy and immunotherapy may have stopped the disease’s progression.
The authors emphasized that because chemo- and immunotherapy are coupled, it is challenging to distinguish between the distinct functions of these anti-tumor-directed therapies on CTD-associated PAH.
“Still, this report suggests that combined chemotherapy and immunotherapy may influence the efficacy of PAH therapies and improve clinical status,” they concluded. “Future clinical investigation is warranted.”